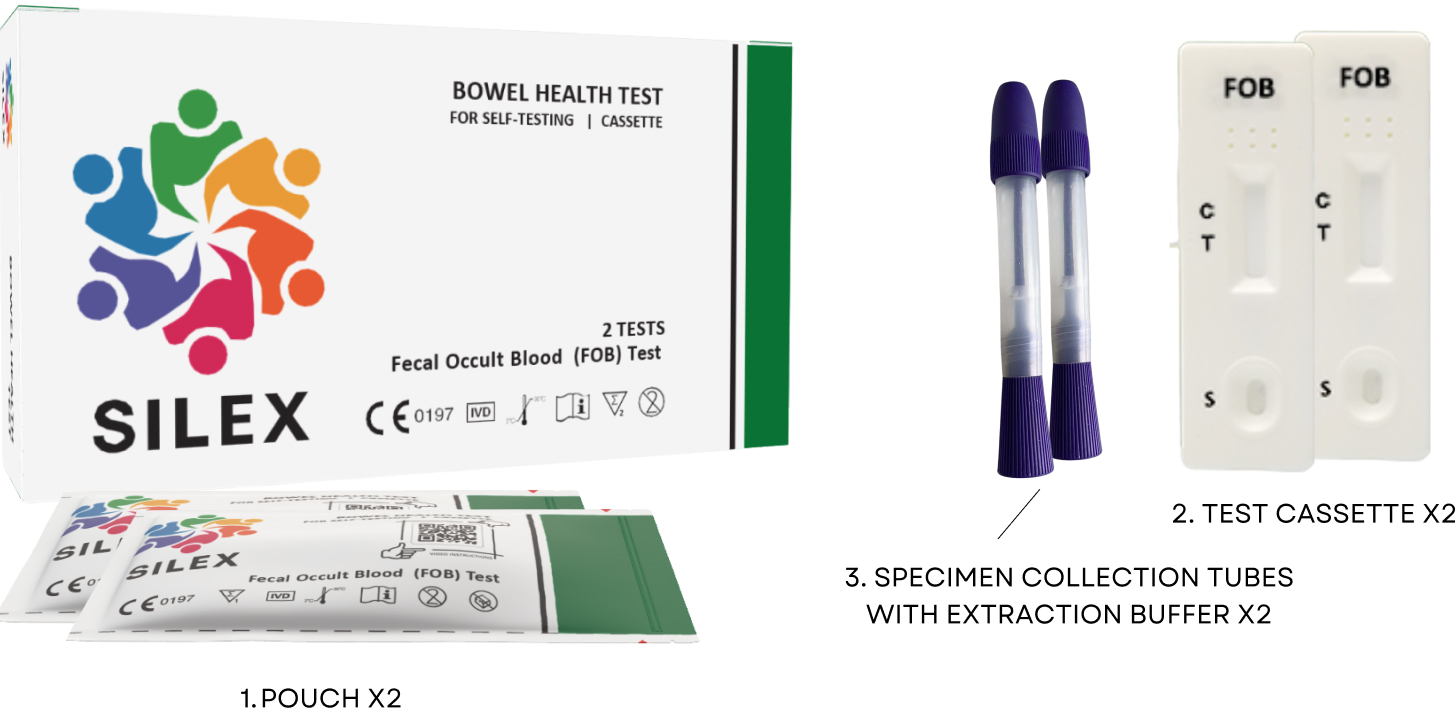
Test Overview
Symptoms
- Change in bowel habits such as passing feces more often or having looser and more runny feces.
- Visible blood in the feces.
- Stomach pain, discomfort or bloating after eating
- Unexpected weight loss - usually 5-10% of your weight in the past 6 months.

FAQs
There are many reasons why you might have blood in your stool. One reason is bowel/colon cancer, however this is not the only reason. Other reasons could be haemorrhoids, diverticular disease, inflammation of the bowel, polyps, stomach ulcers and some medications such as warfarin or aspirin.
- Change in bowel habits such as passing bowel motions more frequently or having looser and more runny motions
- Visible blood in your stool.
- Stomach pain, discomfort or bloating after eating
- Unexpected weight loss - usually 5-10% of your weight in the past 6 months.
- Increasing age - 9/10 bowel cancers occur in those over the age of 50 and 6 out of 10 occur in those over 70.
- Diet - Eating large amounts of red and processed meats can increase your risk of bowel cancer.
- Smoking and alcohol have been shown to increase the risk of bowel cancer.
- Some inflammatory bowel diseases (IBD) such as ulcerative colitis and Crohn’s disease can increase the risk of bowel cancer. (Please note, IBD is different to Irritable bowel syndrome (IBS). IBS does not increase your risk of bowel cancer).
- Some other genetic disorders such as Familial Adenomatous Polyposis (FAP) or Hereditary Non-Polyposis Colorectal Cancer (HNPCC) increase the risk of developing bowel cancer.